The procedure was an ultrasound on his aorta. Walker is ordered to get it every six months.
Chief Investigative Reporter Berkeley Brean: 'So this is something you have to do.'
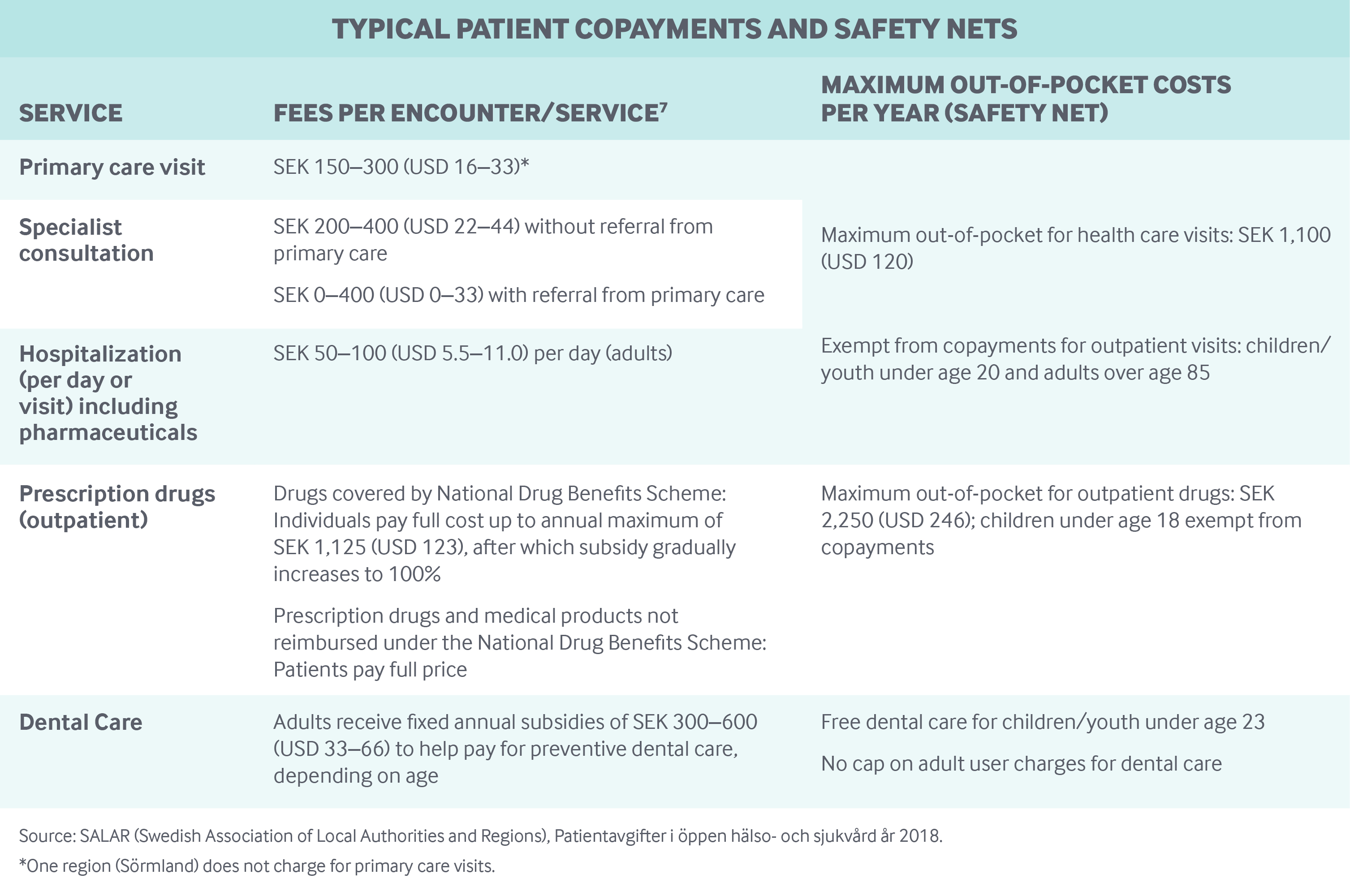
That would depend on your payor. If it is an insurance company that charges copays for preventative care and also E/M visits then you can charage the patient for the two copays. You will be able to tell on your EOB's. There’s no coinsurance, copay or deductible for an annual wellness visit. If the member has had Medicare Part B for more than 12 months, they’re entitled to an annual wellness visit with a primary care provider to develop or update a personalized prevention plan, based on their current health and risk factors.

Ron Walker, two co-pays for one procedure: 'Twice a year. Yeah, I have to do that.'
But here's the issue. Even though he went to one place for one test, Walker ends up getting two bills from UR Medicine for two copays.
One for an office visit. One for a lab visit.
Two Copays For One Office Visit
Re: Billing question - 2 copays for 1 office visit? I agree, that doesn't seem right. Had you seen your regular doctor and had a sonogram, you wouldn't have been charged twice. My eye doctor hit me with two copays, one for his visit and one for a specific test he ran. That didn't seem right, especially as it wasn't explained to me before hand.
Walker: 'That's my complaint. Double copays.'
So for the last couple of days, I've been sharing Walker's problem with UR Medicine. With his permission, I even shared his medical bills. In an email today, UR Medicine Director of External Communications Chip Partner wrote some insurance companies require them to bill for both the procedure and the facility.
Partner's email says 'that is most likely the case here.'
Christopher Bell, Monroe County Medical Society: 'Yeah, I think this is a really good example of the sheer complexity of medical billing.'
Bell is the head of the Monroe County Medical Society.
Brean: 'Shouldn't it be more simple?'
Bell: 'It would be really nice if it were. I think it speaks to the value we hope to see coming out of President Trump's executive order which he signed earlier today.'
Brean: 'Which will do what?'
Bell: 'Well hopefully, among other things it addresses multiple leaders in his cabinet to produce reports with tangible solutions and ways to protect patients from surprise billing as well as better understand the cost that goes into their care.'

The American Medical Association released the following analysis and bullet points of the president's order for more transparency in medical billing.
Multiple Copays For One Visit California
'The purpose of the order is to direct federal agencies to issue regulations to improve the transparency of health care prices and quality in order to create a more competitive marketplace and provide consumers with the information they need to make informed purchasing decisions. More specifically, the executive order:

- Directs the Secretary of Health and Human Services (HHS) to issue regulations within 60 days that would require hospitals to publicly post standard charge information, including information based on negotiated rates, in an easy-to-understand format.
- Requires the Secretaries of HHS, Treasury, and Labor to issue an advance notice of proposed rulemaking within 90 days seeking comment on proposals to require health care providers, insurers, and self-insured group plans to provide consumer access to information about expected out-of-pocket costs before they receive health care services.
- Requires the Secretary of HHS, in consultation with the Attorney General and the Federal Trade Commission, to issue a report within 180 days on ways the federal government or private sector impede health care price and quality transparency for patients, with recommended solutions.
- Directs the Secretary of HHS, within 180 days and in consultation with other federal departments and agencies, to increase access to de-identified claims data from taxpayer-funded health care programs and group health plans for researchers, innovators, providers, and entrepreneurs to facilitate the development of tools that empower patients to be better informed purchasers of care.
- Requires the Secretary of the Treasury, within 180 days, to propose regulations to treat expenses related to certain types of arrangements, potentially including direct primary care and health care sharing ministries, as eligible medical expenses for Health Care Savings Accounts, and to increase the amount of funds in flexible spending accounts that can carry over at the end of the year without penalty.
- Directs the Secretary of HHS to submit a report to the President within 180 days on additional administrative steps that can be taken to address the issue of surprise medical bills.'
The White House also issued a corresponding fact sheet.
Physical therapy is covered to aid in the recovery from disease or injury to help the patient in attaining greater self-sufficiency, mobility and productivity by improving muscle strength, joint motion, coordination, and endurance. Physical therapy is covered when rendered and billed by a licensed, registered physical therapist or other authorized professional provider acting within the scope of his or her license. Professional services performed by a supervised licensed physical therapy assistant (PTA) must be billed under the licensed physical therapist’s National Provider Identification (NPI) number using the CQ modifier. PTAs may not provide an initial examination, evaluation, assessment, or establish a diagnosis or plan of care.
Outpatient therapy is authorized based on one visit per day. All active duty service members (ADSMs), TRICARE Prime and TRICARE Prime Remote beneficiaries who have an assigned primary care manager (PCM) require an approval from Health Net Federal Services, LLC (HNFS) for physical therapy services. TRICARE Prime Remote beneficiaries (excluding ADSMs) without an assigned PCM and TRICARE Select beneficiaries do not require an approval from HNFS prior to services being rendered; however, a physician’s order is required for claims processing.
Coverage is based on the beneficiary's medical needs. The number of visits authorized indicates the actual number of visits, not the individual units per CPT® code. The following baselines will be used as a guide for the number of visits and duration of approval:
- Acute injuries (for example, musculoskeletal conditions such as ankle sprain, shoulder sprain, low back pain or torn hamstring) = 12 visits with a duration of 120 days
- Post-operative care (for example, hip and knee replacement) = 24 visits with a duration of 150 days
- Long term conditions (for example, neurological conditions such as stroke, traumatic brain or spinal cord injury, pediatric neurodevelopmental conditions, swallow testing or feeding therapy) = 72 visits with a duration of 180 days
Individualized Education Program Requirements
Physical therapy to treat a physical or occupational deficiency due to a cognitive or developmental disorder for beneficiaries age three to 21 requires a physician letter of attestation whenever there is evidence presented to TRICARE that there is an individualized education program in place for special education services. TRICARE may cover additional physical therapy when a physician attests in writing the intensity and/or timeliness of any physical therapy services being offered by the educational agency does not meet the medical needs of the beneficiary.
Excluded Services
- diathermy, ultrasound and heat treatments for pulmonary conditions
- general exercise programs
- electrical nerve stimulation used in the treatment of upper motor neuron disorders such as multiple sclerosis
- separate charges for instruction of the patient and family in therapy procedures
- repetitive exercise to improve gait, maintain strength and endurance, and assistive walking such as that provided in support of feeble or unstable patients
- range of motion and passive exercises, which are not related to restoration of a specific loss of function
- maintenance therapy that does not require a skilled level of assistance
- vocational assessment and training or assessments to determine status of disability
- athletic training evaluation (CPT 97005 and 97006)
- CPT 97532 or 97533 when used to improve cognitive function as a result of neuronal growth through the repetitive exercise of neuronal circuits
- CPT 97532 or 97533 for sensory integration training
- services provided to address disorders or conditions resulting from occupational deficits
